The Challenge of Balancing Therapeutic Work and Administrative Responsibility
The challenge of balancing therapeutic work and administrative responsibility is no easy task. As mental health providers, our mental capacity is often tapped out after a few sessions. If you really think about it, the amount of thought and effort placed into a counseling session is intense.
We are actively listening, formulating a working conceptualization, leaning into a theoretical approach, and then facilitating a change mindset to help clients inch closer to their overall goals. We have to think on our feet. We can’t afford distractions. We are 100% focused—energy, attention, and detail—every single session.
Quite honestly, while it’s a beautiful experience, it can also be incredibly exhausting.
Why Progress Notes Feel So Heavy After Sessions
So after a session, the thought of completing a progress note in clinical documentation doesn’t exactly leave us feeling energized. If you’re like many therapists, you may find yourself procrastinating on progress notes, allowing them to pile up until the end of the day—or worse, the end of the week.
And if you think about it, that’s usually when we’re most exhausted.
Yet finding the right balance between clinical work and administrative work is not optional—it’s completely necessary for long-term sustainability in this field.
The Ethical and Professional Responsibility of Documentation
As licensed mental health professionals, we have an ethical, moral, and professional responsibility to keep up with our administrative duties. One of the biggest reasons mental health professionals face complaints, board issues, or malpractice liability often has to do with documentation—or the lack thereof.
We must keep accurate and timely clinical records. This is non-negotiable.
And still, when you’re trying to convince yourself of that reality, a quick break or rushing through the note can feel far more enticing than sitting down to complete documentation thoroughly.
AI, Progress Notes, and Informed Consent
In today’s world of AI, there are supportive tools that can assist with generating session notes. If you choose to go this route, it requires written informed consent from your client. It’s essential that clients fully understand what they’re agreeing to and how their information is being used.
As of 2026, I have personally chosen not to move forward with artificial intelligence in my sessions. I tend to err on the side of caution. I believe we need more time to truly understand AI’s role in therapy—especially when it comes to protecting HIPAA-compliant private health information.
While many platforms claim HIPAA compliance, I work in a field where reliability, integrity, and consistency are often proven over time. Quite frankly, I don’t believe we’ve had enough time yet to determine whether AI-assisted documentation is truly in the best interest of the client.
Structuring Your Schedule for Sustainability
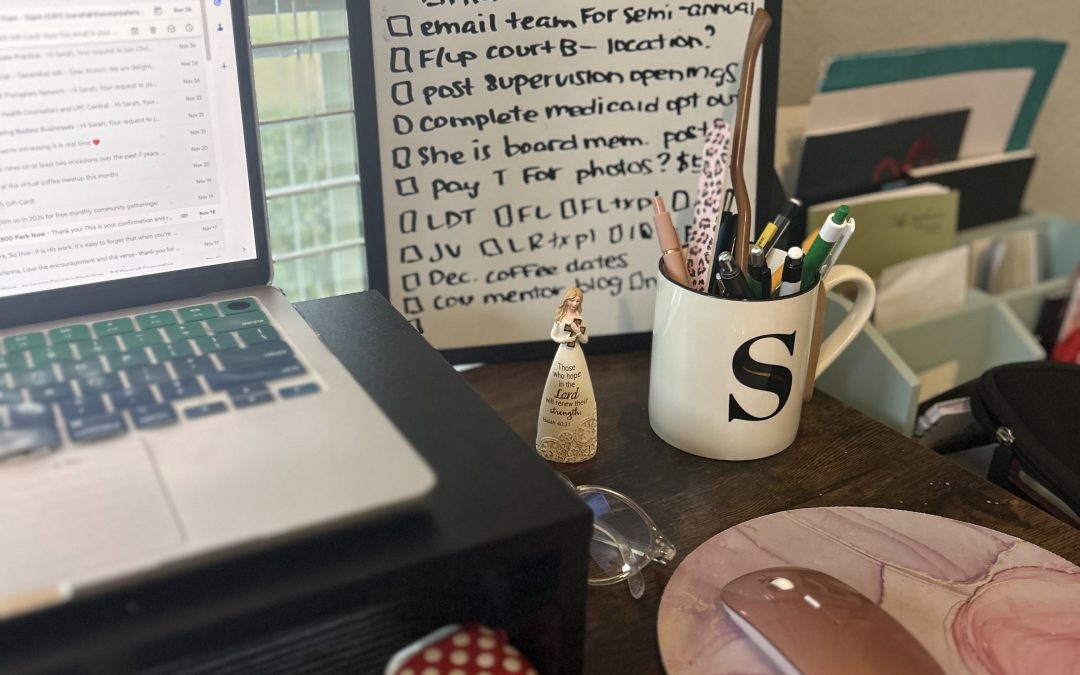
In the meantime, I’ve had to create a structure that works best for me.
A 53-minute session exists for a reason. For those of us working with insurance, that “one-hour session” intentionally allows 7–10 minutes for documentation—if our time management is on point. Of course, this is much easier said than done.
Still, best practice is intentionally prioritizing documentation as close to the session as possible.
The key is knowing your schedule and proactively creating it.
After four back-to-back sessions, I know I need a break. Because of that, I intentionally schedule one-hour breaks on longer clinical days. This allows me to take a 30-minute lunch break and still have at least 30 minutes to complete documentation from earlier sessions.
Time Blocking: A Non-Negotiable Skill for Therapists
Time blocking is absolutely necessary—but it’s something only you can do. If you work in an agency or nonprofit setting, this may require a follow-up conversation with your supervisor to help them understand the strategy behind how you’re structuring your schedule.
Take a look at how many sessions you’re holding each week and clearly identify when documentation will get done. I’m not saying it’s easy—but it is better to establish good habits than to continually break bad ones.
You can do this.